Humana Gold Plus HMO Prior Authorization Form Demystified

Ever feel like healthcare paperwork is a jungle you can't hack through? You're not alone. Many find the world of health insurance, especially something like a "Humana Gold Plus HMO prior authorization form," overwhelming. But don't worry, getting the medical care you need doesn't have to be a Herculean task. Let's break down this process and equip you with the knowledge to navigate it successfully.
The Humana Gold Plus HMO prior authorization form is essentially a request you submit to Humana, asking for approval before receiving certain medical services or prescriptions. It's like getting permission before taking a trip – ensuring your insurance will cover the costs. While it might seem like an extra hurdle, it's designed to help manage costs and ensure you receive appropriate and necessary care. Think of it as a checkpoint to verify that the treatment is medically justified within the plan's guidelines.
Understanding the ins and outs of prior authorization is crucial for anyone enrolled in a Humana Gold Plus HMO plan. Failure to obtain the necessary approvals can lead to unexpected out-of-pocket expenses. No one wants a surprise medical bill, right? This guide will empower you to take control of your healthcare journey and avoid those financial pitfalls. We'll cover everything from what services typically require prior authorization to how to submit the form and track its status.
Navigating the Humana prior authorization landscape might seem daunting initially, but breaking the process down into manageable steps can make it much less intimidating. This involves understanding what the form is, why it's needed, and how to complete it correctly. We'll explore these aspects in detail, ensuring you're well-equipped to handle any prior authorization request that comes your way. You’ll learn how to gather the required information, communicate effectively with your healthcare provider, and follow up on the status of your request.
By the end of this guide, you'll feel confident in your ability to handle the Humana Gold Plus HMO prior authorization process like a pro. You'll know how to submit a complete and accurate authorization request, track its progress, and address any potential issues that may arise. We'll provide tips, tricks, and resources to help you along the way, so you can focus on what matters most – your health.
The history of prior authorization forms is intertwined with the evolution of managed healthcare. As healthcare costs rose, insurance companies implemented these forms to manage expenses and ensure appropriate utilization of resources. The main issue surrounding prior authorizations relates to the potential delay in receiving necessary care while waiting for approval. This can sometimes lead to frustration and anxiety for patients and their families.
A Humana Gold Plus HMO Prior Authorization Form is a document required by Humana for certain medical procedures, tests, or prescriptions. It confirms that the service is medically necessary and covered under your plan. For example, if you need an MRI scan, your doctor would complete a prior authorization form and submit it to Humana for approval before the scan is scheduled.
Advantages and Disadvantages of Prior Authorization
| Advantages | Disadvantages |
|---|---|
| Cost control | Potential treatment delays |
| Ensures appropriate care | Administrative burden |
Frequently Asked Questions
1. What is a prior authorization form? A prior authorization form is a request to your insurance company for approval of a medical service or prescription before you receive it.
2. Why do I need a prior authorization form? Prior authorization ensures the service is medically necessary and covered under your plan.
3. How do I get a prior authorization form? You can usually obtain the form from your doctor's office, Humana's website, or by calling Humana directly.
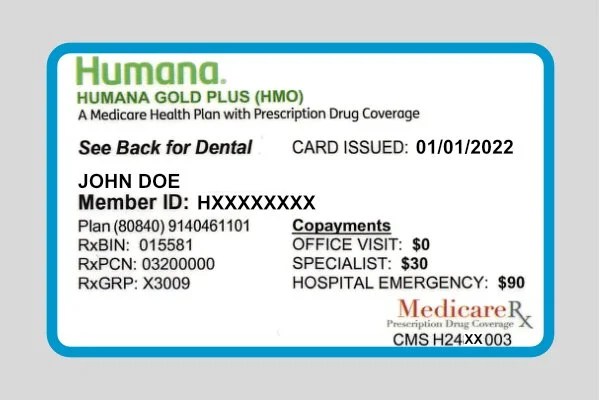
4. What information is needed on the form? Information such as your name, plan information, details about the requested service, and your doctor's information.
5. How long does the prior authorization process take? The process can typically take several business days.
6. What if my prior authorization is denied? You can appeal the decision with Humana.
7. Who submits the prior authorization form? Usually, your healthcare provider will submit the form.
8. How can I check the status of my prior authorization? You can usually check the status online or by contacting Humana.
Tips and tricks: Start the prior authorization process early. Keep records of all communication. Work closely with your healthcare provider.
In conclusion, navigating the Humana Gold Plus HMO prior authorization process doesn't have to be a daunting experience. By understanding the purpose of the form, knowing how to complete it correctly, and working closely with your healthcare provider, you can ensure a smooth and efficient process. Prior authorization plays a vital role in managing healthcare costs and ensuring you receive the most appropriate care. Remember, being proactive and informed empowers you to take control of your healthcare journey. Familiarize yourself with your plan's specific requirements for prior authorization, maintain open communication with your doctor, and don't hesitate to reach out to Humana directly if you have any questions or concerns. This proactive approach will ensure you receive the necessary medical care without any unnecessary delays or financial surprises. Your health is your priority, and understanding your insurance plan is key to maximizing its benefits.
What happens when my brony crew arrives
Versos vsc when your toyotas safety net needs a checkup
Unlocking the secret language of keyboard smiley faces